Table of Contents
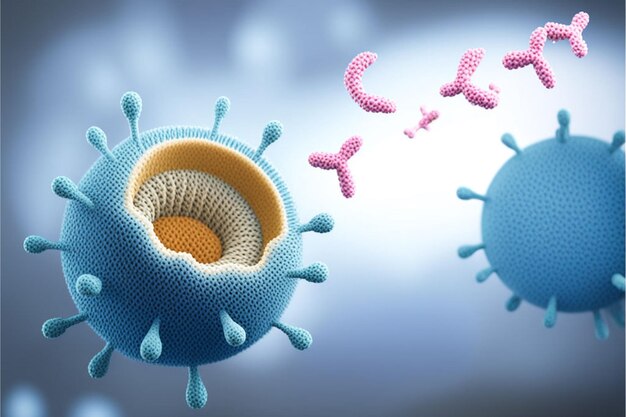
Women and autoimmune disorders: A complex relationship that affects millions worldwide. Did you know that women are significantly more likely to develop autoimmune disorders than men? In fact, nearly 80% of those diagnosed with autoimmune disorders are women. This striking gender disparity in autoimmune disorders has puzzled researchers for decades, prompting extensive studies into why women and autoimmune disorders are so closely linked.
From lupus to rheumatoid arthritis, women and autoimmune disorders share a disproportionate connection. The impact of these conditions on women’s lives cannot be overstated. Women with autoimmune disorders often face unique challenges, balancing their health needs with work, family, and personal aspirations.
Understanding the intricate dance between women and autoimmune disorders is crucial for developing better treatments and support systems. As we delve deeper into the world of women and autoimmune disorders, we’ll explore the latest research, potential causes, and promising breakthroughs.

Women and Autoimmune Disorders: Understanding Their Prevalence
When discussing women and autoimmune disorders, it’s crucial to understand the striking disparity in prevalence between genders. Women and autoimmune disorders are disproportionately linked, with females accounting for nearly 80% of all autoimmune disease cases. This significant association between women and autoimmune disorders has puzzled researchers for decades.Studies focusing on women and autoimmune disorders have consistently shown that females are at a higher risk of developing these conditions compared to their male counterparts.
But why are women more prone to autoimmune disorders? The answer lies in a complex interplay of factors:
1. Hormonal influences
The female sex hormones estrogen and progesterone play a significant role in immune system function. These hormones can enhance the immune response, which may contribute to the increased risk of autoimmune disorders in women.
2. Genetic factors
Some genes on the X chromosome are linked to immune function. Since women have two X chromosomes (compared to one in men), they may have a higher chance of inheriting genes that predispose them to autoimmune disorders.
3. Pregnancy and fetal microchimerism
During pregnancy, fetal cells can persist in a woman’s body for years. These cells may sometimes trigger an autoimmune response, potentially explaining why many women develop autoimmune disorders after childbearing years.
4. Environmental factors
Women may be more susceptible to certain environmental triggers that can initiate autoimmune responses, such as infections, stress, or exposure to toxins.The relationship between women and autoimmune disorders is so pronounced that certain conditions, such as lupus, have a 9:1 female-to-male ratio. The prevalence of women and autoimmune disorders varies across different conditions. For instance, women are two to three times more likely to develop multiple sclerosis, and they make up 90% of all systemic lupus erythematosus cases.
Understanding the prevalence of women and autoimmune disorders is not just about recognizing statistics. It’s about acknowledging the unique health challenges that women face and the need for targeted research and healthcare approaches. The high prevalence of women and autoimmune disorders underscores the importance of early screening, diagnosis, and treatment specifically tailored to women’s health needs.
As research on women and autoimmune disorders continues to evolve, scientists are exploring these various factors that might explain the gender disparity. By delving deeper into the connection between women and autoimmune disorders, researchers hope to develop more effective prevention strategies and treatments that address the specific needs of women living with these chronic conditions.

Common Autoimmune Disorders Affecting Women
When it comes to women and autoimmune disorders, several conditions stand out due to their prevalence and impact. Let’s explore some of the most common autoimmune disorders that disproportionately affect women:
Lupus
Systemic Lupus Erythematosus (SLE) is often called the “great imitator” due to its varied symptoms that can mimic other diseases. This condition primarily affects women, with a striking 9:1 female-to-male ratio. Lupus can impact multiple organs, causing symptoms ranging from joint pain and skin rashes to organ damage. The iconic “butterfly rash” across the cheeks and nose is a telltale sign of this complex disorder.
Rheumatoid Arthritis
More Than Just Joint Pain. While many associate arthritis with aging, rheumatoid arthritis (RA) is an autoimmune condition that can strike at any age. Women are 2-3 times more likely to develop RA than men. This disorder goes beyond joint pain – it can cause fatigue, fever, and in severe cases, affect the heart and lungs. The symmetrical nature of joint involvement (affecting the same joints on both sides of the body) is a distinctive feature of RA.
Hashimoto’s Thyroiditis
The Silent Thyroid Attacker. This condition is the most common cause of hypothyroidism in areas with sufficient iodine intake. Hashimoto’s thyroiditis affects women 5-10 times more often than men. It’s a sneaky disorder, often developing slowly over years. Symptoms can be subtle at first – fatigue, weight gain, and depression – making it easy to overlook until the thyroid is significantly damaged.
Multiple Sclerosis
Multiple Sclerosis (MS) is a condition where the immune system attacks the protective covering of nerves. Women are three times more likely to develop MS than men. This disorder can cause a wide array of symptoms, from vision problems and fatigue to mobility issues. Interestingly, pregnancy can often provide temporary relief from MS symptoms, highlighting the complex relationship between hormones and autoimmune disorders.
Celiac Disease
Not Just a Food Trend. While gluten-free diets have become trendy, for those with celiac disease, it’s a medical necessity. This autoimmune disorder, triggered by gluten consumption, affects the small intestine and can lead to malnutrition if left untreated. Women are diagnosed with celiac disease two to three times more often than men. Symptoms can range from digestive issues to seemingly unrelated problems like anemia or osteoporosis.
Understanding these common autoimmune disorders affecting women is crucial for early detection and treatment. Many of these conditions share overlapping symptoms, which can make diagnosis challenging. However, being aware of the increased risk and common signs can empower women to seek medical attention early, potentially leading to better management and outcomes.It’s important to note that while these disorders are more common in women, they can affect anyone. The key takeaway is to listen to your body, be aware of persistent or unusual symptoms, and don’t hesitate to discuss concerns with healthcare providers. Early intervention in autoimmune disorders can often lead to better quality of life and reduced complications.
Hormonal Influences on Autoimmune Disease Development
The intricate dance between hormones and the immune system plays a crucial role in the development of autoimmune disorders in women. When exploring women and autoimmune disorders, we cannot overlook the significant impact of hormonal fluctuations throughout a woman’s life.
Estrogen, often dubbed the “female hormone,” is a key player in the story of women and autoimmune disorders. This hormone can enhance immune responses, which is a double-edged sword. While it may offer women stronger protection against certain infections, it also increases the risk of the immune system turning against the body’s own tissues. This hormonal influence partly explains why women and autoimmune disorders are so closely linked. Interestingly, the relationship between women and autoimmune disorders often shifts during pregnancy. Some conditions, like rheumatoid arthritis, may improve during pregnancy, while others, such as lupus, might flare up. This phenomenon highlights the complex interplay between hormones and autoimmune activity in women.

The onset of puberty, menstrual cycles, pregnancy, and menopause – all hormone-driven events – can trigger or exacerbate autoimmune disorders in women. For instance, many women with multiple sclerosis experience symptom changes that correlate with their menstrual cycles, further emphasizing the connection between women and autoimmune disorders. Understanding these hormonal influences is crucial for both patients and healthcare providers. For women with autoimmune disorders, tracking hormonal changes and their impact on symptoms can be an empowering tool for managing their condition. Healthcare professionals treating women with autoimmune disorders often consider hormonal factors when developing treatment plans, recognizing that the approach to these conditions in women may need to be different from that in men.
Research into the hormonal aspects of women and autoimmune disorders is ongoing and promising. Scientists hope that by unraveling these complex relationships, we can develop more targeted treatments and perhaps even preventive strategies for women at risk of autoimmune diseases. In conclusion, the hormonal factor is a fascinating piece of the puzzle when it comes to women and autoimmune disorders. It underscores the need for a nuanced, gender-specific approach to understanding, diagnosing, and treating these conditions in women.
Diagnosis Challenges and Delayed Treatment for Women
The journey of women and autoimmune disorders is often marked by a winding path to diagnosis. Despite the higher prevalence of autoimmune conditions in women, the road to proper identification and treatment can be frustratingly long and complex.One of the primary challenges in diagnosing women and autoimmune disorders lies in the nature of the symptoms. Many autoimmune conditions present with vague, non-specific symptoms like fatigue, joint pain, or skin rashes. These symptoms can easily be dismissed or misattributed to stress, hormonal changes, or other common ailments.
Consequently, women and autoimmune disorders often face a significant delay between the onset of symptoms and a correct diagnosis.The medical community’s understanding of women and autoimmune disorders has historically been limited, leading to potential biases in diagnosis. Some healthcare providers may be less likely to consider autoimmune conditions when evaluating women’s health complaints, particularly if the symptoms don’t fit neatly into a specific disease pattern. This knowledge gap can result in women and autoimmune disorders being overlooked or misdiagnosed.

Another factor complicating the diagnosis of women and autoimmune disorders is the overlap of symptoms between different autoimmune conditions. For instance, fatigue and joint pain can be symptoms of lupus, rheumatoid arthritis, or fibromyalgia, among others. This overlap can lead to a lengthy process of elimination before arriving at the correct diagnosis.The impact of delayed diagnosis on women and autoimmune disorders cannot be overstated. Early detection and treatment are crucial for managing these conditions effectively and preventing long-term damage. Unfortunately, many women report feeling dismissed or not taken seriously when reporting their symptoms, further delaying proper care.
To address these challenges, it’s essential to raise awareness about women and autoimmune disorders among both healthcare providers and the general public. Encouraging open communication between patients and doctors, promoting comprehensive testing, and validating women’s health concerns can all contribute to more timely diagnoses.For women experiencing persistent, unexplained symptoms, it’s crucial to be proactive advocates for their health. Keeping detailed symptom journals, seeking second opinions when necessary, and requesting autoimmune-specific testing can all help in navigating the complex landscape of women and autoimmune disorders.
While diagnostic challenges persist for women and autoimmune disorders, increased awareness and advocacy are slowly improving the situation. By understanding these challenges, both patients and healthcare providers can work together to ensure more timely and accurate diagnoses for women facing autoimmune conditions.
Managing Autoimmune Disorders: Lifestyle and Treatment Options for Women
When it comes to women and autoimmune disorders, management is key to maintaining a good quality of life. While there’s no one-size-fits-all approach, a combination of medical treatments and lifestyle modifications can help women effectively manage their conditions.

Medical Treatments
For women and autoimmune disorders, treatment often involves medications that suppress or modulate the immune system. These may include:
– Immunosuppressants
– Biologics
– Corticosteroids
– Disease-modifying antirheumatic drugs (DMARDs)
The choice of medication depends on the specific autoimmune disorder and its severity. Women and autoimmune disorders require personalized treatment plans, often involving a team of specialists.
Lifestyle Modifications
Beyond medication, lifestyle changes play a crucial role in managing autoimmune disorders in women:
- Diet: Some women with autoimmune disorders find relief through anti-inflammatory diets. While dietary needs vary, many benefit from reducing processed foods and increasing intake of fruits, vegetables, and omega-3 fatty acids.
- Exercise: Regular, moderate exercise can help manage symptoms and improve overall well-being for women with autoimmune disorders. Activities like yoga, swimming, or walking are often recommended.
- Stress Management: Stress can trigger flare-ups in women with autoimmune disorders. Techniques such as meditation, deep breathing exercises, or counseling can be beneficial.
- Adequate Rest: For women with autoimmune disorders, getting enough sleep and rest is crucial for managing fatigue and supporting the immune system.
- Support Networks: Connecting with other women who have autoimmune disorders can provide emotional support and practical tips for daily living.

Holistic Approaches
Some women with autoimmune disorders find complementary therapies helpful, such as acupuncture, massage, or herbal supplements. However, it’s important to discuss these with a healthcare provider to ensure they don’t interfere with other treatments.
Monitoring and Adjusting
Women and autoimmune disorders often require ongoing monitoring. Regular check-ups and lab tests help track the progression of the disease and the effectiveness of treatments. Treatment plans may need adjusting over time as the condition or life circumstances change.
Pregnancy Considerations
For women with autoimmune disorders who are considering pregnancy, special planning is often necessary. Some medications may need to be adjusted or changed before and during pregnancy to ensure the safety of both mother and baby. In conclusion, while living with an autoimmune disorder presents challenges, many women successfully manage their conditions through a combination of medical treatments and lifestyle adjustments. The key is working closely with healthcare providers to develop a personalized management plan that addresses the unique needs of women with autoimmune disorders.